Pneumonia is a serious lung infection that is particularly dangerous for the elderly as it weakens the immune system and decreases lung function. The disease is the second leading cause for hospitalization of Medicare beneficiaries, and its complications can be fatal, especially for seniors.
Pneumonia is a lung infection that can be dangerous for senior citizens. While people of all ages can contract it, older adults with weakened immune systems are at increased risk.
This disease progresses quickly with poor outcomes for the elderly. If hospitalization is required, these individuals are at a higher risk of developing complications and requiring lengthy hospital stays.
The American Lung Association reports that 85% of deaths from pneumonia and influenza occur in people over 65. The disease has a 20% mortality rate in this age group, where it is the seventh leading cause of death.
What Is Pneumonia
Pneumonia is an infection of the lungs that causes fluid or pus to develop in the alveoli (air sacs). This makes it difficult to breathe and hard for the exchange of oxygen in your blood.
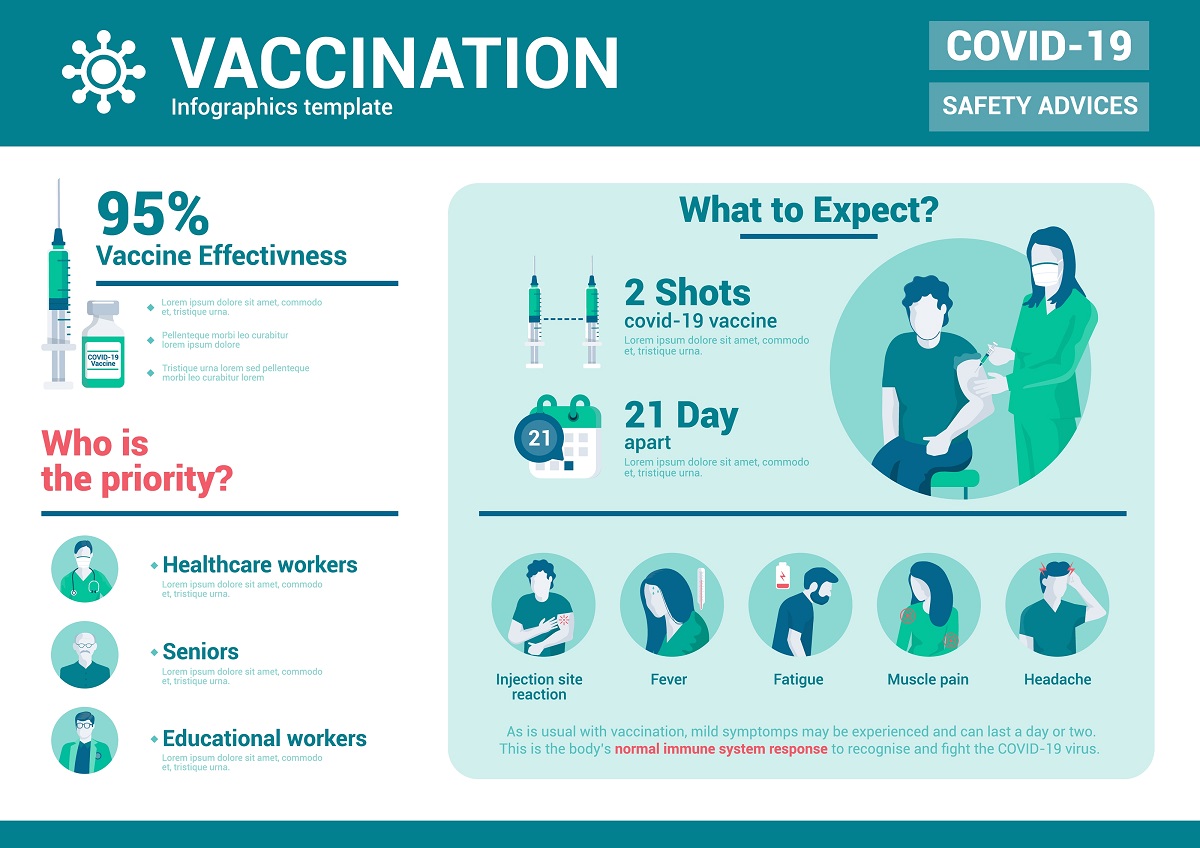
The disease can be caused by a virus, a bacteria, or a fungus. The virus that causes Covid-19 can cause pneumonia, which is why getting Covid vaccines and boosters is highly recommended for seniors!
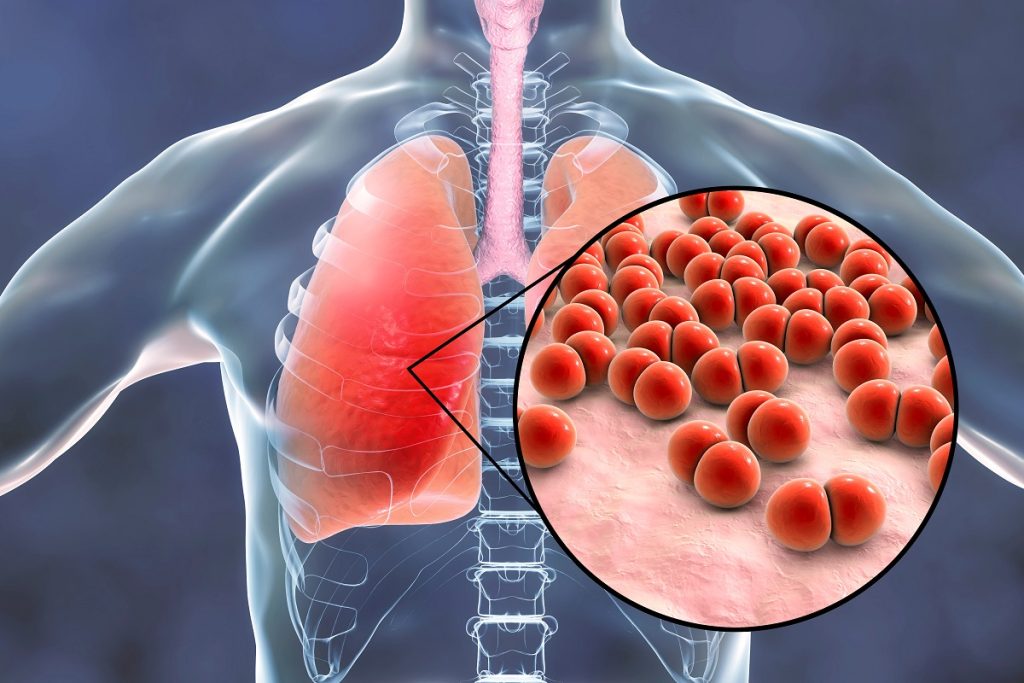
The most common cause of CAP is Streptococcus pneumonia. Older adults are at an increased risk of developing pneumonia due to the following:
- A weakened immune system
- Comorbidities
- Decreased cough reflex
- Decreased ability to perform activities of daily living (ADL)
There are several types of pneumonia that particularly attack the elderly. Community-acquired pneumonia (CAP) causes around 1 million cases of pneumonia in elderly individuals (>65 years of age) per year in the U.S. This type of pneumonia is acquired outside of a hospital, nursing home, or healthcare facility.
Those in facilities are at risk of other forms of pneumonia:
- Hospital-acquired pneumonia
- Healthcare-associated pneumonia
- Ventilator-associated pneumonia
- Aspiration pneumonia
Why Is It So Dangerous For The Elderly?
Pneumonia is dangerous for the elderly population because of their increased risks (weakened immune system, comorbidities, and decreased cough reflexes) which can lead to severe pneumonia.
The primary cause of death for the 20% who succumb to severe pneumonia is respiratory insufficiency. This is when the lungs cannot meet the oxygen and carbon dioxide needs of the cells in your body.
What Are The Symptoms Of Pneumonia In the Elderly?
Although older adults’ symptoms are atypical, they can consist of:
- Shortness of breath (dyspnea)
- Lack of appetite
- Urinary incontinence
- No fever to lower than normal body temperature
- Change in their ability to perform ADLs
- Feelings of weakness and unsteadiness
- Confusion
The subtlety of these symptoms puts the elderly population at high risk for delayed diagnosis and treatment.
Other typical symptoms are fever and chills, a productive cough (where phlegm is produced), chest pain, fatigue, and rapid breathing.

What Happens When The Elderly Get Pneumonia?
Usually, we filter germs with our breath. If germs enter our lungs, our body’s immune system goes into action. This process could cause inflammation and fluids and pus to form in the alveoli (air sacs) as a by-product, resulting in pneumonia.
When an elderly individual gets pneumonia, per the Mayo Clinic, the causes of pneumonia depend on where they got it and the bacteria, virus, or fungus that caused it.
Community-acquired pneumonia (CAP), the most common type of pneumonia, can be caused by:
- Bacteria (the most common in the U.S. is Streptococcus pneumoniae)
- Bacteria-like organism (Mycoplasma pneumoniae known as walking pneumonia)
- Fungi (common amongst individuals with chronic health problems and weakened immune systems)
- Viruses (usually cause mild pneumonia, but the Coronavirus may cause pneumonia to be severe)
Hospital-acquired pneumonia (HAP) is acquired during a hospital stay and is more severe due to the bacteria being resistant to antibiotics and the person’s decreased immune system. It is common for people in the intensive care unit (ICU) to be on ventilators (breathing machines).
Healthcare-associated pneumonia occurs when an individual is in a nursing home or receiving care at an outpatient clinic (i.e., a kidney dialysis facility). Like HAP, this type of pneumonia can be challenging due to the person’s immune system and the drug-resistant bacteria.
Aspiration pneumonia happens when an older adult has weakened gag reflexes or swallowing issues, inhaling food, drinks, vomit, or saliva into their lungs.
The bacteria and viruses that cause pneumonia in the community are different from those that cause pneumonia in healthcare settings. Because many people in this age group have a reduced ability to cough, culturing their sputum may be difficult.
How Serious Is Pneumonia For Elderly Patients?
Pneumonia in the elderly population is a very serious concern. This is why early detection and treatment are important. Signs that you and your loved ones can look for are:
- Chest pain
- Bluish coloring of your nails, lips, or face
- Changes in mental status
- Difficulty breathing
- Abnormal body temperature
Some risk factors include:
- Chronic lung diseases (chronic obstructive pulmonary disease (COPD), Cystic fibrosis, and bronchiectasis)
- Smoking
- Chronic illnesses (heart disease, diabetes, and sickle cell anemia)
- Recent viral respiratory infection (a cold, COVID, and flu)
- Alcohol and drug abuse
- Hospitalization
- Exposure to chemicals and toxins
- Weakened immune system

So, prevention is key!
Older adults aged 65 and older should get the Pneumococcal vaccine, the Hib (Haemophilus influenzae type b) vaccine, the Coronavirus vaccine, and a yearly Flu (influenza) vaccine. Also, wash your hands, eat smaller meals, make sure you are getting enough rest, and quit smoking.
Because even with treatment, pneumonia can lead to serious complications.
How Can Pneumonia Be Treated In The Elderly?
The treatment of pneumonia for older adults is dependent on the cause of the infection,
- Viral pneumonia
- Bacterial pneumonia
- Fungal pneumonia
- Aspiration pneumonia
Viral pneumonia treatment usually consists of supportive therapy. But, antivirals may be given depending on the type of virus. If viral pneumonia is caused by the flu (influenza), then Tamiflu will be given.
For bacterial pneumonia, an antibiotic may be given specifically for the type of bacteria causing the infection based on its severity. You may feel good after 1 to 3 days of starting the antibiotic, but you must finish the course of antibiotics because the infection can return.
The treatment of fungal pneumonia is with antifungal medications.
Aspiration pneumonia is mainly treated with antibiotics, and the medication of choice relies upon where the incident happened and if you have a penicillin allergy.
Both hospital-acquired pneumonia and healthcare-associated pneumonia are often treated with different antibiotics than those used for bacterial pneumonia due to being caused by an antibiotic-resistant strain.
But, it is common for pneumonia to be treated outpatient with supportive therapy requiring:
- Rest
- Fever reducers (ibuprofen and acetaminophen)
- Fluids
- Oxygen therapy
- Hot beverages/broths and humidifiers
- Cough medications are recommended only if you are having trouble sleeping because coughing is the best mechanism for getting secretions out of the lungs.
Only severe cases require hospitalization from complications such as abnormal heart rate, blood pressure, body temperature, respiratory failure, and confusion.

Can An Elderly Person Survive Pneumonia?
An elderly person can survive pneumonia. That is why early detection and diagnosis are imperative.
When they present to their Primary Care Provider (PCP), the doctor will evaluate the individual’s health condition and determine which tests are needed.
They may order a chest x-ray, coronavirus test, and blood test and check your oxygen levels with pulse oximetry.
If you are in the hospital and your condition is severe, the doctor may order:
- An arterial blood gas to measure the oxygen in the blood.
- A CT scan for a more detailed look at the lungs.
- Blood culture to determine what pathogen is the cause and see if the infection has spread to the blood.
- Sputum culture to identify the germ that is causing the infection.
- A polymerase chain reaction (PCR) test to check the DNA of the sputum or blood to find the germ.
- A bronchoscopy to look inside your airways and possibly collect tissue and fluid samples to classify the germ.
- A pleural fluid culture, known as a thoracentesis, is used to collect fluid from the pleural (the area between your chest and lungs) to test for bacteria.
All of these steps are performed to decrease an elderly patient’s incidence of respiratory distress, bacteremia, sepsis, use of a mechanical ventilator, lung abscess, and death. So, if your symptoms are not improving, follow up with your PCP for further testing.

